Immunoglobulin G (IgG) serves as one of the body’s primary defenses against infections, playing a crucial role in the immune system’s function. However, when IgG levels fall below normal ranges, it can pave the way for various health complications. In this comprehensive guide, we delve into the intricate relationship between low IgG levels and the development of diseases, shedding light on the underlying mechanisms, diagnostic approaches, and treatment options.
Unraveling the Role of IgG in Immune Function
- Understanding Immunoglobulin G (IgG): IgG constitutes a significant portion of the body’s antibodies, playing a pivotal role in immune response modulation.
- Functions of IgG: IgG antibodies facilitate the recognition and neutralization of pathogens, thereby preventing infections and bolstering immune defense mechanisms.
- Immune Surveillance: IgG antibodies contribute to immune surveillance by identifying and targeting foreign invaders, such as bacteria, viruses, and other pathogens.
- Importance of IgG Levels: Maintaining optimal IgG levels is essential for sustaining immune function and protecting against infectious diseases.
Low IgG Levels: Causes and Consequences

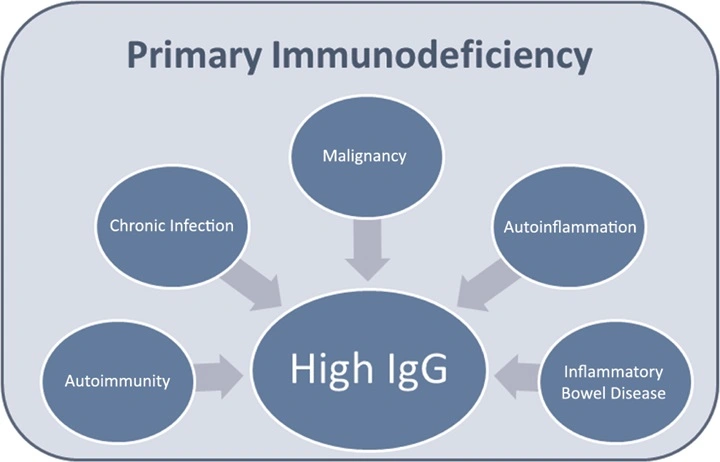
- Primary Immunodeficiency Disorders: Genetic mutations or abnormalities can lead to primary immunodeficiency disorders, characterized by decreased IgG production and susceptibility to recurrent infections.
- Secondary Immunodeficiency: Various factors, including chronic illnesses, medications, and certain medical treatments, can contribute to secondary immunodeficiency, resulting in diminished IgG levels and compromised immune function.
- Consequences of Low IgG: Reduced IgG levels increase the risk of recurrent infections, autoimmune disorders, and other health complications, highlighting the significance of timely diagnosis and intervention.
Diseases Associated with Low IgG Levels
3.1 Respiratory Infections
- Pneumonia: Individuals with low IgG levels are more susceptible to bacterial pneumonia, leading to severe respiratory symptoms and potential complications.
- Sinusitis: Chronic sinusitis can occur due to recurrent infections in individuals with compromised immune function, often characterized by persistent nasal congestion and facial pain.
- Bronchitis: Low IgG levels predispose individuals to recurrent episodes of bronchitis, accompanied by coughing, chest discomfort, and difficulty breathing.
3.2 Gastrointestinal Disorders
- Inflammatory Bowel Disease (IBD): Low IgG levels have been implicated in the pathogenesis of IBD, including Crohn’s disease and ulcerative colitis, contributing to chronic inflammation and tissue damage in the gastrointestinal tract.
- Infectious Diarrhea: Diminished IgG levels compromise gut immunity, increasing susceptibility to various pathogens responsible for infectious diarrhea, such as norovirus, rotavirus, and bacterial agents.
3.3 Autoimmune Disorders
- Rheumatoid Arthritis (RA): Low IgG levels are associated with an increased risk of autoimmune disorders like RA, characterized by chronic joint inflammation, pain, and progressive joint damage.
- Systemic Lupus Erythematosus (SLE): Dysregulated immune responses, including decreased IgG levels, contribute to the development of SLE, a multisystem autoimmune disorder with diverse clinical manifestations.
3.4 Neurological Conditions
- Multiple Sclerosis (MS): Emerging evidence suggests a potential link between low IgG levels and the pathogenesis of MS, a chronic autoimmune disease affecting the central nervous system and causing neurological deficits.
- Guillain-Barré Syndrome (GBS): Reduced IgG levels may predispose individuals to GBS, a rare autoimmune disorder characterized by acute peripheral nerve inflammation, muscle weakness, and paralysis.
Diagnostic Evaluation of Low IgG Levels
- Laboratory Testing: Serum IgG levels can be measured through blood tests, providing valuable insights into immune status and identifying potential deficiencies.
- Immunological Assays: Immunological assays, such as enzyme-linked immunosorbent assay (ELISA) and immunofluorescence, help quantify IgG levels and assess immune function.
- Differential Diagnosis: Differential diagnosis involves ruling out other causes of immunodeficiency and investigating underlying conditions contributing to low IgG levels.
Management Strategies for Low IgG-Associated Diseases
- Immunoglobulin Replacement Therapy: Intravenous or subcutaneous immunoglobulin administration helps replenish IgG levels, enhance immune function, and reduce the risk of infections in individuals with immunodeficiency disorders.
- Disease-Specific Treatments: Targeted therapies, including anti-inflammatory agents, immunosuppressants, and disease-modifying drugs, are utilized in managing autoimmune disorders and mitigating disease progression.
- Supportive Care Measures: Adopting preventive measures, such as vaccination, infection control practices, and lifestyle modifications, plays a crucial role in optimizing health outcomes and minimizing disease-related complications.
Empowering Health through Understanding and Intervention
In conclusion, the association between low IgG levels and diseases underscores the importance of immune surveillance and maintenance of optimal immunoglobulin levels in safeguarding against health threats. By elucidating the intricate interplay between immune function and disease pathogenesis, healthcare providers can implement timely interventions and personalized treatment approaches to improve patient outcomes and enhance overall well-being. Through ongoing research efforts and advancements in diagnostic modalities and therapeutic interventions, the management of low IgG-associated diseases continues to evolve, offering hope for better prognosis and quality of life for affected individuals.